In 2002, the body of the American football player, Mike Webster, arrived at an autopsy table at the University of Pittsburgh, USA. At the time, the immigrant pathologist from Nigeria, Bennett Omalu, was responsible for the autopsy. Webster had died after years of suffering with cognitive and intellectual disabilities, mood disorders, drug abuse and poverty as well, and although Webster's brain appeared normal at the autopsy, Omalu decided to conduct further analyzes on a few tissues from the famous player's brain. .
The university did not agree to Omalu's request; As the additional tests will cost thousands of dollars, for the Nigerian doctor to decide to pay for them from his own pocket, Omalu believed that the American football player suffers from a type of dementia called boxing dementia, a form of dementia caused by repeated blows to the head, and indeed, The man partially validated his assumption; Later, he published a set of studies stating that American football is a game of great danger to the brain. Repeated collisions that occur during play cause severe and irreversible damage to the brain, damage that kills players after they suffer bad torment of delusions and turn their lives into a nightmare. delusions; Before the player died, he experienced symptoms including delusion, hearing non-existent voices, and neurological disorders that may be classified as schizophrenic symptoms.
A relentless battle was waged against "Omalo", the parties to which were the game union in the United States of America and its fans thirsty for fun and excitement and fanatical for its teams that support it, but he decided to stand in the face of the flood, and proved beyond any doubt the correctness of his claim, which gave him the qualities of heroism and granted him A degree of fame, and years later, specifically in 2015, the famous American actor, Will Smith, presented the life story of the Nigerian doctor "Omalu" in an iconic movie called "Concussion".
Omalu has proven that American football players who are subjected to severe friction and severe shocks frequently during consecutive sports matches can develop serious neurological diseases, but, what if you suffer a single minor or moderate injury to your brain, can you That affect you for the rest of your life? The results of a recent study published in the journal "Science" indicate that this is very likely, not only have we established the possibility of neurodegenerative effects from moderate-severity injuries, but the researchers also identified the molecule responsible for these secondary effects of what is known as traumatic injury, and were able to find A method that prevents the action of that molecule.
Brain injuries are divided into several types, the first of which is a mild injury, which does not cause a prolonged loss of consciousness, but the patient shows signs of confusion and temporary memory loss. A severe injury is one that causes the casualty to lose consciousness for more than 6 hours.
traumatic brain injury
When a person is traumatized by a fall from a flight of stairs, a car accident, or even a large book falling on the head from a library, they often recover, but years after the injury they may have difficulty sleeping and become very sensitive to noise or bright lights. He may also find it difficult to perform his daily activities or to function well. This is very common after a traumatic brain injury, also known as a traumatic brain injury; People can have bad side effects months or years later, and these effects can also last long-term, extending from a few days into the rest of a person's life.
Traffic accidents are the most common cause of TBI, then sports and physical activities come in second place, and physical assaults rank third, and for the elderly, falling is the first cause of TBI.
Traumatic brain injury (TBI) is a major cause of disability in children and adults. It affects about 69 million people worldwide each year and can lead to cognitive dysfunction, difficulty in sensory processing (malfunctioning and integrating data from the different sensory organs), sleep disturbance, and epileptic seizures.
According to the study, most of these adverse outcomes appear months or years after traumatic brain injury, and are caused by indirect secondary injuries that develop as a result of the primary impact. Since the primary injury is essentially irreversible, understanding where, when, and how secondary injuries develop is critical to preventing Disability or treatment after traumatic brain injury.
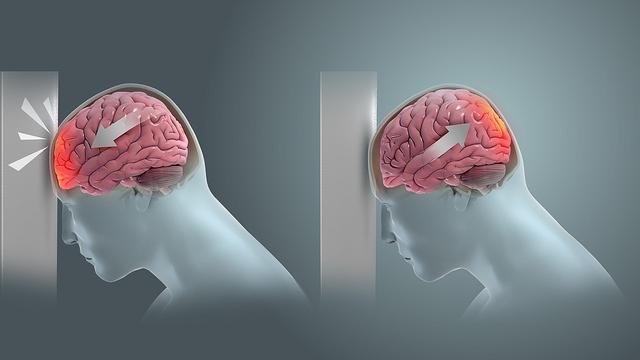
Although the cerebral cortex may be the primary site of injury, the thalamus (the middle area between the two equal halves of the brain, between the cerebral cortex and the midbrain) may suffer secondary injury after TBI, presumably due to the existence of a mutual connection between the cortex The superficial layer of the brain and the thalamus are a large mass of gray matter.
chronic neurodegeneration
Secondary injuries in the hypothalamus lead to significant changes in the neurons, and cause inflammation that may result in chronic neurodegeneration, and usually, most attempts to get rid of this inflammation fail, which leads to non-reversible damage to the nerve circuits, that is, it cannot be reversed by therapeutic means. This is a major cause of neurodegenerative diseases.
So far, there are no treatments to prevent the disabilities that can develop after brain trauma, so understanding how traumatic injuries affect the brain, especially in the long term, can help heal a cognitive rift that may in turn help develop new treatment options that are relevant. A stronger impact repairs the damage from the initial shock.
In that study, researchers helped bridge that gap, having identified a specific molecule in the hypothalamus that plays a key role in secondary effects of brain injury, such as sleep disturbance, epileptic activity and inflammation, but also showed that antibody therapy can prevent the development of these negative outcomes.
The main goal of this study was to understand how the brain changes after a traumatic injury, and how these changes can lead to chronic problems, such as the development of epilepsy, sleep disturbance and difficulty in sensory processing, which include disorders that affect one of the five senses or More than that, it may also mean motion sickness and difficulty waking up, or avoiding crowds and crowded places.
To do this, the scientific team recorded the activity of different cells and neural circuits in the brains of mice after brain injury. The researchers constantly monitored the mice after they attached electrodes to their brains that transmitted brain activity wirelessly. This means that mice can go about their normal activities without being disrupted.
Using this method, the team was able to collect a lot of data during the injury and over the next several months, to find that during a head injury, an area of the brain called the cortex is often the primary site of injury. Because it is located directly under the skull.
However, according to the study's author, Gianna Baz, in exclusive statements to "the science", this mild injury moved from the cortex to the deeper brain structure, "the thalamus was more affected than the cortex itself," which "represented a great surprise to us." ".
But how can a site far from the primary trauma - the thalamus - be affected more than the primary site - the cerebral cortex?
That's due to an inflammatory molecule known as C1Q, Gianna says, which the researchers found "highest levels in the hypothalamus."

Scientists have known about this molecule for a long time. It is a protein complex that is part of the innate immune system. This molecule binds to antigens and helps create an inflammatory response that enables the body to fight bacteria, but like all components of the immune system, it is a double-edged sword.
The C1Q molecule is part of the immune pathway and has a well-documented role in normal brain development and function, for example, it protects the central nervous system from infection and helps the brain forget memories—a process necessary for storing new memories. The accumulation of C1Q in the brain has been studied in many It is a neurological and psychiatric disorder, and is associated - for example - with Alzheimer's disease and schizophrenia.
Just as immunity protects us from pathogens, it can cause severe damage to the body, which is the case in all kinds of immune diseases, in which immunity attacks the body and internal organs, and sometimes destroys them.
sleep spinners
The researchers in that study wanted to find a way to block the harmful effect of this molecule, but without affecting its beneficial role.
“With increased levels of this molecule in the brain, an inflammatory response occurs that leads to degenerative diseases,” Paz says, noting that it takes “several years, during which this molecule engages with the immune system to attack the neural structure, especially in the hypothalamus.” This leads to impaired function of brain circuits and death of neurons.
The researchers say the thalamus appears to be "particularly vulnerable after TBI," which does not mean, of course, that the cortex will not be affected by increased levels of C1Q, but simply that it "has unknown tools for recovery over time, unlike the thalamus."
Chronic brain injury and neuronal loss include a range of diseases, chief among which are sleep disturbances and abnormal brain activity such as seizures, but the news isn't all bad.
Mice with chronic brain injury, when treated with new therapeutic antibodies that block a specific inflammatory pathway, “reduced all of the symptoms we observed, lower levels of inflammation and minimal neuronal loss, and the mice regained their ability to sleep, and epileptic seizures decreased.” Baz told Al-Ilm.
To validate their findings, the researchers examined human brain tissue and found that brains with past traumatic injuries had high levels of the same molecule.
When the researchers studied mice genetically engineered to lack C1Q at the time of shock, brain injury appeared much worse. In the first place it has a very harmful effect, but it can be prevented after injury to reduce harmful inflammatory responses in the brain,” says Paz.
In addition to the chronic inflammation, the scientific team detected abnormal brain activity in mice with TBI; Researchers have observed disturbances in sleep spindles, which are normal brain waves or rhythms that occur during sleep and last from half a second to two seconds, an important process for strengthening memory. of normal cognition and behaviour, and they also indicate a greater susceptibility to seizures.
Antibody therapy
The scientists noted that treatment with antibodies known as anti-C1Q anxon inhibitors not only helped restore sleep spindles, but also prevented the development of epilepsy activities.
Anti-anxon inhibitors are a type of antibody that treats many autoimmune and neurological disorders, and they are already used in a range of medications that have been shown to be safe for humans.
Overall, the study suggests that targeting the C1Q molecule after injury can prevent some of the most devastating long-term consequences of TBI, and the researchers hope this will eventually lead to the development of treatments for TBI.
Baz says that it may take months or years for many of the adverse health outcomes that can result from brain injury to appear, and “the reasons behind this are not known precisely,” but she points out that the study of chronic neuritis as one of the possible mechanisms for the deterioration of Cognitive function after traumatic brain injury "may yield very good results in the design of drugs to be prescribed to human subjects."
Associate Professor at the Institute of Global Health and the Environment at American University, Mohamed Salama, a researcher who has been working on neurodegenerative diseases for years, says: The study confirms that “mild injuries are associated with degenerative diseases,” noting that this type of injury - “especially in the case of recurrence.” It is seen as one of the factors leading to these diseases.
Salama notes that this scientific paper “represents a very important entry point for determining the relationship between traumatic injuries and degenerative diseases,” noting that “many studies are needed to lay strong foundations to fully clarify this relationship.”
Baz totally agrees with Salama; In her statements to Al-Alam, she says that the study "focuses on one hypothesis, and there may be many other causes of chronic cognitive impairment after brain injury." Rather, the researcher stresses the need to be careful about applying this knowledge on a large scale in the treatment of sleep disorders or epilepsy; "Both conditions have many different etiologies, and in addition to the mechanisms we identified in our study, this means that there may be many different approaches to drug development, depending on the underlying causes of the disorder."
Although there are currently no treatments available for these injuries, Paz says that in most cases, symptoms improve with rest and time, "but it is difficult to predict whether a brain injury will lead to other neurological problems, and therefore almost impossible to prevent."
The study author stresses that the best way to protect against brain injury is to prevent injury; She advises everyone to wear protective equipment such as helmets and seat belts, "Make your home safe by reducing trip hazards, and install protective equipment in accident-prone locations, such as stairs and windows."
